Forum Replies Created
-
AuthorPosts
-
 Keith TaylorParticipant
Keith TaylorParticipant
If I were you I would follow nobody’s advice and start allopurinol as soon as possible. As for diet be very careful what you read. Because protein from plants and low-fat dairy is good for gout. As you eat little meat I think you would be very happy with a Mediterranean diet. But don’t include processed foods with additives like sugar.
It’s not too complicated really. But confusing if you read rubbish from people who don’t understand gout. So if you want good opinions it’s better to tell us where you read rubbish about spinach and legumes. Because then I can explain why they are good for you and where the others got it wrong.
 Keith TaylorParticipant
Keith TaylorParticipantHi Diane,
I’m sorry, but I have more questions than answers at the moment. Because I don’t have enough information to help you properly. So, can you tell me:
1. When were you first diagnosed with gout.
2. When did you start taking allopurinol?
3. Are your 2 allopurinol tablets 100mg or 300mg?
4. Have you taken different doses of allopurinol in the past? If so, what doses and when did they change.
5. Do you have exact uric acid test results and approximate dates?
6. Have you ever taken any other gout pain relief besides prednisone?Thanks
 Keith TaylorParticipant
Keith TaylorParticipantOn the chances of repair d_q, it seems to depend on the type of damage caused. Because I found a relevant 2014 report below.
The report deals with extreme
goutUric Acid Arthritis, and extreme uric acid lowering. So, it doesn’t exactly match your situation. But I believe the principles still apply. So there’s strong evidence to suggest bone erosion will repair itself. Unfortunately, less chance of Joint Space Narrowing reversal, or cartilage repair.Joint Repair after Uric Acid Lowering Reference
Dalbeth, Nicola, Anthony J. Doyle, Fiona M. McQueen, John Sundy, and Herbert SB Baraf. “Exploratory Study of Radiographic Change in Patients With TophaceousGoutUric Acid Arthritis Treated With Intensive Urate‐Lowering Therapy.” Arthritis care & research 66, no. 1 (2014): 82-85. Bone Erosion Reversed after Uric Acid Lowering PDF. Keith TaylorParticipant
Keith TaylorParticipantNo More Gout!
That’s the last time I use the G-Word – at least for today. Because the only way to stop it forever is to change the way we look at it.
Urate Crystal Arthritis is so easy to cure, you don’t even need help from a website. 😉
Here is a new way to stop gout. Much more than a name change. Urate Crystal Arthritis is easy to control. See how to control uric acid arthritis today.
 Keith TaylorParticipant
Keith TaylorParticipantHey nobody, I never said it was a good joke! Also, I put high school to widen the audience. Because, of course, I went to grammar school – a haven for puerile humour. Just say “I like a mass debate” out loud. It was very funny when I was 13.
Granted, less funny now. 🙂
 Keith TaylorParticipant
Keith TaylorParticipantIt was certainly my intention to keep the focus of this on getting mobile quickly during acute inflammation. So, please accept my apologies if I’ve appeared to be talking about habitual exercise during inter-critical bouts.
Perhaps it’s best to add “woolly-brained and fuzzy-focused” to the list. Also, something about weak wanker humor as the “mass debate” joke never raised a trace of laughter.
Anyway, I think the perfect solution is d_q’s “I think in future if an attack does strike I will take the more relaxed approach rather than express mobility.”
I.e. it’s up to each individual to act according to their own beliefs. Now, I realize that’s not very scientific. But, I can now see that there is no reliable science to determine the best course of action. So, if you believe rest is the answer, then it probably is. And if you believe getting mobile as soon as possible is the answer, then it probably is.
Because until we have a proper medical study on human gout sufferers, we cannot say which is best. Also, I imagine that even if this is done, it will always depend on several complicated mitigating factors. For example, what if mobility increases immediate pain, with no lasting damage, but quicker recovery from the acute flare? Then that’s OK with me because I can tolerate that pain. But a different gout sufferer might not find this acceptable.
Finally, I can see the start of at least 2 more fascinating topics here.
First is d_q’s interesting way of getting what he wants from his rheumatologist and what happens next. The second, perhaps related, is the merits of MRI vs Ultrasound. Though returning to hedging my bets, I have to agree with nobody that it depends on what you are looking for.
 Keith TaylorParticipant
Keith TaylorParticipantPersonally, I think the relationship of gout to bones is the same wherever they are located. Because uric acid crystals will eventually lead to bone damage in and around affected joints. So, assuming your uric acid is still under control, I’d put this down to minor discomfort from old crystals dissolving. But, if it continues, you should see your doctor with it to rule out any other damage.
The foot is always complicated when it comes to gout. Because there are many conditions that get confused with gout. Especially complicated where these conditions co-exist. So I will continue to add specifics about this particular problem in my Sesamoiditis versus Gout explanations. As a general rule, I’ve noted that the best approach is usually to get uric acid safe. Then you can focus on sesamoids, bunions, or other bone or cartilage defects if they continue once gout is resolved.
 Keith TaylorParticipant
Keith TaylorParticipantI suppose it’s inevitable that costs get mentioned when Krystexxa is discussed. But, as a life-saving treatment for unresponsive gout, it’s more of a moral issue than a gout issue. Personally, I think the best place to discuss medical costs is outside this gout forum. Because it’s political, not medical.
Anyway, when I posted this message from the Feedback form, I hoped to introduce the topic of Krystexxa. So, it’s fantastic to see John’s update. I understand what nobody means when he says “If I thought Tophus Sufferer would read this thread, I’d have brought up pegloticase myself.” Because it seems futile to respond to questions that are unlikely to get reactions from the original poster. But, I tend to think of the thousands of visitors who don’t feel comfortable posting to forums. Because they will get good knowledge from seeing the real-life benefits of extreme tophi control.
So, thanks to all who contributed here. I think I have some more relevant Krystexxa information somewhere. So, I hope to dig it out soon.
 Keith TaylorParticipant
Keith TaylorParticipant“I’d be interesting in knowing the opinion of your current rheuma.”
So would I. But, I’m looking for a specific opinion on whether mobility helps inflammation or not.To explain, I’ve caused confusion between:
-habitual exercise (that is, when you’re NOT having an acute attack… and I do mean “acute” as opposed to whatever you might have that lasts for months)
-exercise during an attack
-weight-bearing exercise involving a joint affected by an attackI believe habitual exercise is a separate topic. Specifically: “But, please note this is not about the general benefits of exercise for gout sufferers. Because I should already have explained that at Gout & Exercise.”
But, I do think I could have been clearer about the other points.
To explain, I do not want to encourage gout sufferers to risk further damage to joints that have already been weakened through gout. So, if you suspect this is the case, you should get imaging tests immediately. Certainly, standard X-rays and ultrasound are useful. But, if funding is available, then CAT scans or MRI scans reveal a better picture.
As an aside, let’s look at that damage for a moment. Because uric acid crystals cannot cause “mechanical damage” in the way I understand the meaning. Uric acid crystals cause tendinitis, osteoarthritis, and other damage through the immune response system. That is to say, when white blood cells (WBCs) attack uric acid crystals, all hell breaks loose. Because our bodies rely on many different types of WBCs. Some of which were destined to repair bone, cartilage, etc.
So, there is no mechanical wearing down of joints. But, lack of maintenance because the janitors have been sacrificed to battle.
I think that this is a separate topic. Unless forced mobility of inflamed joints increases the chances of more specialist WBCs being sacrificed. Which means we have one meaningful question to ask a rheumatologist:
“Is there any evidence to support the notion that osteoblasts, tenocytes, and other specialized cells are at risk if mobility is increased during periods of inflammation” ❓
Finally, I return to my suggestion that mobility can reduce the duration of inflammation where there is no indication of joint damage. So, my second question for d_q’s rheumy is:
“Please can you explain Pinto’s reasons for recommending “sit less and move more”, particularly light-intensity activities and/or breaking-up sedentary time.” ❓Because that is key to understanding mobility during gout attacks.
Of course, the real issue remains to get uric acid controlled. Then, gout stops and none of this matters. But like d_q, I love a good debate. Which is why I proposed the Mass Debating Society in high school. 😉
 Keith TaylorParticipant
Keith TaylorParticipantYou suspect right, nobody, except it is sweetened with cane sugar. But like you say, it’s better to get used to unsweetened cereals. In particular, these breakfast biscuits are widely available in the original 100% whole wheat versions (delicious with a moderate serving of real fruit). In this case, Ron even got the name wrong! Because it’s Kashi Autumn Wheat: https://www.amazon.com/Kashi-Organic-Promise-Cereal-Biscuits/dp/B001E5E06U
7g of sugar per recommended serving, which probably means more like 12g. That is approx one-quarter of the recommended daily sugar intake.
“Will that hurt my gout?” Oh yes! But personally, I’d worry more about heart disease and diabetes than dying of gout.
To all Gout Foodies write out 100 times:
“Of course the amounts you eat matters more than the exact product. And what matters [most] is your whole diet.“ Keith TaylorParticipant
Keith TaylorParticipantYeah, good weekend thanks. But not so good as last weeks family garden party for my sisters birthday. These events get better as the generations grow. : grin:
Anyway, let me explain my thoughts and investigations so far about mobility during an acute gout flare.
Firstly, for the thousands of gout sufferers who will read this in future, let me summarize the background. Because this starts with my approach to acute gout pain management. Where I stated:
First and foremost I had an epiphany when I realized gout pain stems from an immune reaction. Prior to that, I had the more typical view that sharp uric acid crystals were forming. So, I understood the importance of getting mobile as soon as possible. Fortunately, prescription strength ibuprofen (Aleve) kept me going almost every time. But if it didn’t I supplemented with paracetamol (Tylenol).
So, I’m explaining my approach in an acute gout flare setting. But I also want to explain the science. Then gout patients can explain to their doctors why they need the right pain treatment to stay mobile during acute attacks. Because in my experience, you get a better response when you ask your doctors opinion about a specific medical study. Compared to “some bloke on the Internet says…”
Eventually, I want to incorporate this into the facts and templates on my main gout website. So, here’s some work-in-progress. But, please note this is not about the general benefits of exercise for gout sufferers. Because I should already have explained that at Gout & Exercise. Though, I can see that needs some updating after 6 years.
Acute gout pain is an inflammatory immune system response to uric acid crystals
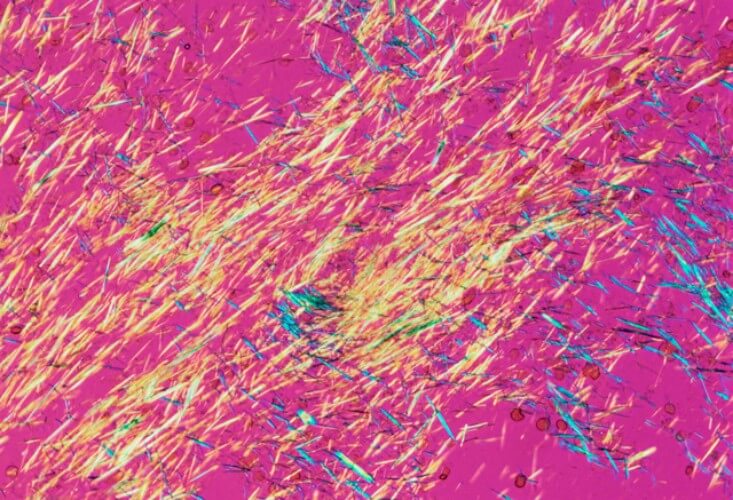
I’m emphasizing this as my starting point. Because I still see references to uric acid crystals as “sharp needle-like”. But this is nonsense as it describes objects at a microscopic level which cannot be sharp. Also, to describe them as needle-like is like describing grains of soft sand as “craggy boulder-like”.Unfortunately, this led me in the wrong direction as a newbie gout sufferer. Because I thought I should avoid more physical damage from these “sharp” crystals and rest as much as possible. But I couldn’t understand why attacks lasted more than a week in bed. Yet, if I had to force myself to work I was OK in 2-3 days.
Medical approach to inflammation
Before I get to the science of inflammation, I must point out I cannot find any specific investigations into the effect of mobility on gout flare duration. So, I have looked at inflammation in general. But, I’m aware that some aspects of specific diseases might mean we cannot apply certain findings to gout. Therefore, if you are looking for exact gout science about mobility during acute gout, please leave now. Perhaps you can raise funds for specific research. Or experiment on yourself. In any case, I can only give some strong pointers that remaining mobile is best.Half a century ago, the attitude to inflammation was rest and immobilization. So Partridge’s 1963 arthritis study[1] advocates
a period of complete immobilization can safely be used in the treatment of rheumatoid arthritis to control pain, muscle spasm, and disease activity.
But, this contrasts completely with Pinto’s 2017 investigation[2]:
make the patients “sit less and move more”, particularly light-intensity activities and/or breaking-up sedentary time, is a simple and prudent therapeutic approach to minimize physical inactivity and sedentary behavior, which are overlooked yet modifiable risk factors in the field of autoimmune rheumatic diseases
So now, I’m trying to understand what are the specific inflammatory factors that mean mobility is beneficial during acute gout. Because I think there are specific gout-related factors behind Pinto’s recommendation.
Most recently, I’m looking at Wood’s 2009 investigation[3]. In turn, that has me frying my brain with Bruunsgaard’s 2005 explanation of physical activity and inflammation[4]. To explain “frying my brain”, I understand half the keywords: “myokines; TNF-alpha; IL-6; proinflammatory; antiinflammatory; exercise”. But, I think there’s real scope for a clear explanation. Because many of the terms in this study look like terms in complicated gout pain studies (which also fry my brain)
Practical Advice
Let’s assume I can convince the world that for acute gout flares, mobility is best. Then I hear the next question: “But I have a desk job, so I can’t stay active”. Well, I tripped over the answer in Bort-Roig’s 2014 study[5]. “17 tips for mobilizing gout recovery” Coming Soon!And now you know why I never find time to answer forum questions promptly! 😮
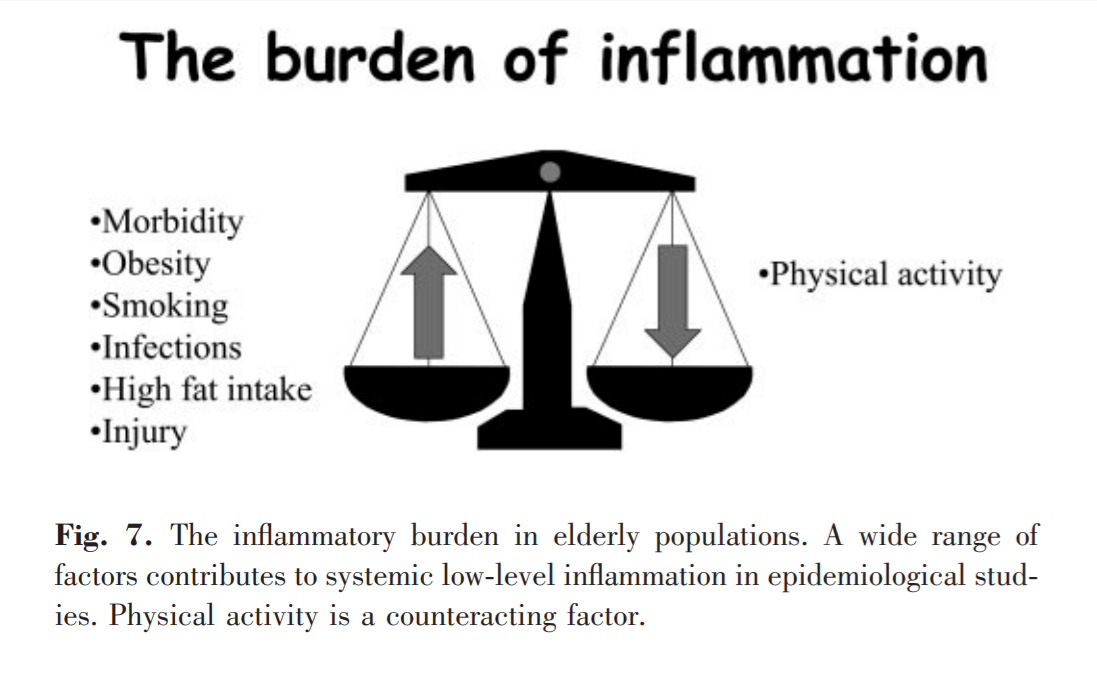
High Fat Meals cause Gouty Inflammation – Physical Activity reduces it
Mobility During Gout Flare References
- Partridge, R. E. H., and J. J. R. Duthie. “Controlled trial of the effect of complete immobilization of the joints in rheumatoid arthritis.” Annals of the Rheumatic Diseases 22.2 (1963): 91.
- Pinto, Ana Jéssica, et al. “Physical inactivity and sedentary behavior: Overlooked risk factors in autoimmune rheumatic diseases?.” Autoimmunity Reviews (2017). Ask if you need a PDF. Because I need to dive into my pocket for it.
- Woods, Jeffrey A., Victoria J. Vieira, and K. Todd Keylock. “Exercise, inflammation, and innate immunity.” Immunology and allergy clinics of North America 29.2 (2009): 381-393.
- Bruunsgaard, Helle. “Physical activity and modulation of systemic low-level inflammation.” Journal of leukocyte biology 78.4 (2005): 819-835.
- Bort-Roig, Judit, et al. “Uptake and factors that influence the use of ‘sit less, move more’occupational intervention strategies in Spanish office employees.” International Journal of Behavioral Nutrition and Physical Activity 11.1 (2014): 152
 Keith TaylorParticipant
Keith TaylorParticipantThanks, Andy – I need to make a couple of points:
1. 6 months may not be long enough. Keep careful records of uric acid levels and gout flares. Consider yourself safe when you have gone 6 months without a gout flare, and with uric acid at 5 or below. Get monthly tests for uric acid, kidney function, and liver function. Uric Acid Test frequency can be relaxed when results stabilize, but never less than once a year.
2. My advice is not professional. It is here to help you discuss gout with your own professional medical team, and is no substitute for visiting your doctor. There may well be circumstances in your medical history or family history that make my advice bad. I usually describe myself as a layman. A better word might be amateur – I do it for love, but it is vital that you discuss my advice with your doctor.
 Keith TaylorParticipant
Keith TaylorParticipant7 is not safe for anyone who has ever had gout. You are almost certain to end in a state where uric acid crystals dissolve and reform, sending continuous signals to your immune system. White blood cells attack crystals in both these states, and it is difficult to tell from the pain. Attacks during crystals dissolving tend to be more widespread, but this is not always the case.
The target for most gout sufferers is 5 mg/dL (0.30 mmol/L).
This might need to be relaxed to 6 if kidney problems or other health issues prevent attaining 5, but 5 gives the best safety margin for fluctuations in uric acid level, and in temperature.
It is always a good idea for the first six months to try to get down to 2 or 3. This dissolves existing crystals faster. Which reduces the period of time you are at risk from gout flares.
 Keith TaylorParticipant
Keith TaylorParticipantHi Andy,
“during that 2 months, the uric acid was keeping below 4, I assume that crystal has been removed in my body”
I think the problem is time. 2 months is not really long enough to get rid of old crystals. They grow very slowly, so if you noticed 2 years ago, they will have started long before that. Some dissolve quite quickly, but others are trapped behind dead white blood cells.
I always regard 6 months as the minimum time for getting rid of crystals. You did the right thing by increasing febuxostat, but I think you should have kept that going longer. Of course, there is always the chance that your recent pain is something other than gout, so if it persists, it’s better to get it checked.
 Keith TaylorParticipant
Keith TaylorParticipantSushi is no different from any other type of cuisine. To tackle gout, you have to start from a basically healthy diet. That means avoiding excesses of calories, iron, and animal purines. It does not mean avoiding these completely – just eat a sensible amount. Every person’s needs are different, so you might ask for personal help in the forum. Before you do, I urge you to read my Gout Foods guidelines.
Because of this, there is no specific advice on sushi. However, I did mention sushi in Octopus and Gout. Also, see Gout Foods Table for Fish.
 Keith TaylorParticipant
Keith TaylorParticipantHi Vanessa, you need to think about your whole diet. Individual foods are not really important until you consider how they fit with everything else you eat.
Eating crawfish every day is bad for you. That’s not a gout thing, it’s just bad diet. Because, it leads to lots of health problems, not just gout. So, consider eating fish once or twice a week. Also, oily fish is better, like salmon. So, mix it up, with occasional crawfish along with other fish.
Because gout is suspected, you should get regular uric acid tests. So, ask your doctor how frequently you should get tested. Then you get a clearer picture about your gout, and how to treat it. As it isn’t too high, we might be able to control your gout with better diet. Just let me know if you want me to help you plan a healthy gout diet.
 Keith TaylorParticipant
Keith TaylorParticipantThen, I’ll amend or expand relevant existing articles.
And, so far, those articles are:
- Gout And Alcohol
- What Is The Best Alcoholic Beverage To Drink With Gout?
- Allopurinol And Alcohol: Can You Spirit Away Gout?
- Foods High in Uric Acid.
I’m sure there are others, so please add them below, as you find them. Thanks.

Beer and gout comic courtesy The Brewery Comic
-
AuthorPosts